Guide to Managing Pet Arthritis Pain
Dietary Considerations for Pets with Arthritis
Nutritional Needs of Different Pet Types
Every pet has unique dietary requirements that directly impact their health and vitality. Canines and felines, for instance, have fundamentally distinct nutritional needs. Canines thrive on meals packed with high-quality protein and complex carbs to fuel their active lifestyles and maintain lean muscle mass. Felines, being true carnivores, demand meat-based diets rich in taurine and other essential nutrients found only in animal tissues. These species-specific requirements make it imperative to select food formulas designed for each animal type.
Importance of High-Quality Protein
Premium protein sources form the foundation of optimal pet nutrition, supporting everything from tissue repair to immune defense. When evaluating pet foods, prioritize those featuring whole meat sources as primary ingredients. Options like free-range poultry, grass-fed beef, and wild-caught fish deliver complete amino acid profiles that promote vitality. Insufficient protein intake can manifest in concerning ways - muscle wasting, slower wound healing, and increased susceptibility to illness being among the most noticeable.
Managing Weight and Obesity
Excess weight creates unnecessary strain on a pet's joints and organs, potentially shortening their lifespan. Overweight animals face heightened risks for debilitating conditions like osteoarthritis and cardiovascular disease. Implementing measured meal portions alongside consistent activity routines forms the cornerstone of successful weight control. Many pet owners find success with specially formulated weight management diets that provide satiety while controlling caloric density. Remember, gradual weight loss (1-3% of body weight weekly) proves safest for long-term success.
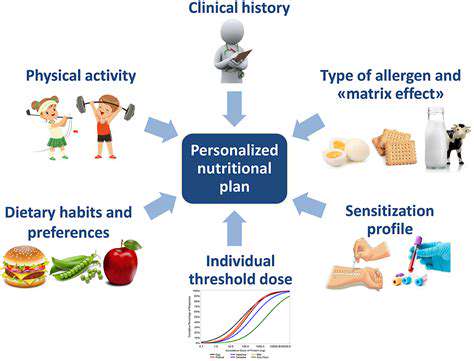
Addressing Specific Dietary Allergies and Sensitivities
Food intolerances can significantly diminish a pet's quality of life, often presenting as chronic skin irritation or digestive upset. The most prevalent triggers include common fillers like corn, wheat, and soy, along with certain animal proteins. Elimination diets supervised by a veterinary nutritionist remain the gold standard for pinpointing problematic ingredients. Novel protein sources such as venison or duck, paired with easily digestible carbohydrates like sweet potatoes, frequently resolve these dietary challenges.
Supplements and Special Diets
Targeted nutrition becomes increasingly important as pets age or develop health conditions. Mature companions often show remarkable improvement when transitioned to diets enhanced with glucosamine, chondroitin, and omega-3 fatty acids for joint support. Pets with renal issues may require phosphorus-restricted formulas, while cardiac patients often benefit from sodium-controlled options. These therapeutic diets work best when implemented under veterinary guidance, with regular progress monitoring.
Effective Pain Management Strategies
Understanding the Different Types of Pain
Pain manifests in diverse forms, each requiring distinct intervention approaches. Acute pain typically signals immediate tissue damage, while chronic pain persists beyond normal healing timelines. Neuropathic pain arises from nervous system dysfunction, presenting as burning or tingling sensations, whereas nociceptive pain stems from actual or potential tissue injury.
Accurate pain assessment forms the foundation of effective treatment, necessitating thorough evaluation of its quality, radiation patterns, and aggravating/alleviating factors. This diagnostic clarity enables healthcare providers to match interventions to the pain's underlying mechanisms.
Pharmacological Pain Management Options
Modern medicine offers a spectrum of analgesic options tailored to pain severity and origin. NSAIDs like carprofen work well for inflammatory pain, while opioids remain reserved for severe acute episodes. Novel approaches like gabapentinoids effectively manage neuropathic components, and local anesthetics can provide targeted relief when administered via nerve blocks.
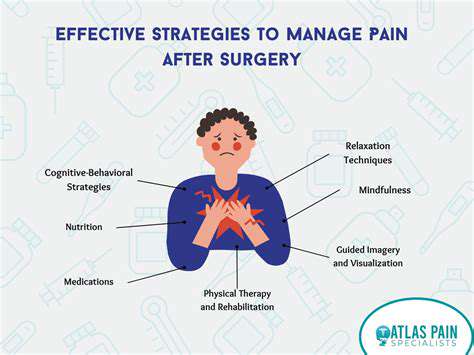
Non-Pharmacological Pain Management Techniques
Multimodal approaches often yield superior results compared to medication alone. Customized physical therapy regimens can restore functional movement patterns while simultaneously decreasing discomfort through therapeutic exercises and manual techniques. Aquatic therapy proves particularly beneficial for arthritic patients, allowing movement with reduced joint loading.
Thermal modalities (alternating heat and cold applications) modulate pain signals, while mindfulness-based stress reduction techniques help patients develop healthier relationships with persistent discomfort.
Lifestyle Modifications for Pain Management
Daily habits significantly influence pain perception and tolerance. Anti-inflammatory nutrition emphasizing omega-3 fatty acids, turmeric, and antioxidant-rich produce creates an internal environment less conducive to pain signaling. Consistent sleep hygiene practices and strategic pacing of activities prevent the boom-bust cycles that exacerbate chronic pain conditions. Even gentle movement practices like tai chi demonstrate measurable benefits for pain sufferers.
Complementary and Alternative Therapies
Integrative modalities expand the pain management toolbox considerably. Medical acupuncture stimulates endogenous opioid release, while therapeutic massage improves circulation and reduces muscle guarding. Evidence continues to accumulate for certain botanicals like devil's claw and white willow bark in mild to moderate pain management.
These approaches work best as part of comprehensive care plans developed in collaboration with licensed healthcare providers familiar with both conventional and complementary medicine.
The Importance of Patient Education and Support
Knowledge transforms patients from passive recipients to active participants in their care. Understanding pain neuroscience helps individuals reinterpret sensations and employ coping strategies more effectively. Peer support groups provide validation and practical tips for navigating daily challenges.
Multidisciplinary pain rehabilitation programs that combine medical management with psychological support and functional restoration demonstrate particularly strong outcomes for complex chronic pain cases. This holistic approach addresses the biological, psychological, and social dimensions of persistent pain.
Read more about Guide to Managing Pet Arthritis Pain
Hot Recommendations
- Review: [Specific Brand] Small Animal Cage
- Why Rescuing Pets Saves Lives
- Best Pet First Aid Kits [What to Include]
- How to Help Stray Animals in Your Community
- Guide to Adopting a Pet When You Have Kids
- Top Reptile Heat Lamps
- Heartwarming Rescue Stories That Will Inspire You
- Review: [Specific Brand] Bird Cage
- Best Aquarium Filters [2025 Review]
- Review: [Specific Brand] Smart Litter Box




![My Experience Rescuing a Small Animal [Story]](/static/images/33/2025-05/AJourneyHomeandCaringfortheTinyTraveler.jpg)
![Review: The [Specific Brand] Smart Pet Feeder](/static/images/33/2025-05/ConnectivityandAppIntegration3AASeamlessExperience3F.jpg)
![Top Harnesses for Dogs That Pull [Review]](/static/images/33/2025-06/Top-RatedHarnessesforEffectiveControl.jpg)
